Histopathology
Hi all. For the past 2 weeks, I was attached to the Histopathology lab. Basically the lab does routine work everyday: tissue processing, embedding, microtomy, etc. Of all, trimming can be considered the most interesting process, we will be able to see different tissues such as placenta and tonsils being cut. For every process, it is very crucial that the initial of the staff performing the job is indicated to facilitate traceability, as any small error may result in the wrong diagnosis.
Ok now I shall let you have an idea of how a Histopathology lab works. Following are the procedures that I observe everyday:
Receiving of Specimens – When specimens are first obtained at the lab, the information on the container/plastic bag (patient name/nature of specimen) must be checked against the requisition form. Next, the time and date is recorded and the medtech who performed the check will sign a form for the staff who sent in the specimens to prove the receipt. Labels which contain a barcode unique for every patient will then be printed and stick to the form and the specimen.
Most specimens sent in are fixed in formalin, which hardens the tissue for easy trimming. Large specimens are usually fixed overnight before trimming to ensure that formalin penetrates into all parts of the specimen. In the lab, formalin prepared would be sufficient for one week use.
Trimming and Passing – Before trimming of some large specimens such as breasts, asst pathologists will dye the specimen with different colored dyes to indicate the margins. While trimming, they will dictate the measurements and observations seen on the specimen (eg. a tumor measuring 2cm by 2cm is seen at 7 o’clock position) and these are immediately typed out by a lab assistant who sits just beside the asst pathologist. These observations would be printed out, attached with the requisition form and sent to pathologists to make the diagnosis. They will cut certain parts of the specimen where they suspect an abnormality may be present and ‘pass’ them into cassettes labeled with the patient number and year. For small samples, the number of strips of tissue will be written on the cassette to ensure that the embedder removes every single piece of tissue. Gel is also used to clump all the small strips of tissues together. Cassettes are labeled using a special marker which is resistant to formalin and other reagents. Also, different colored cassettes are used for different cases. All the cassettes are then placed into the automated tissue processor which works overnight, to perform thorough fixation as well as dehydration to remove all water from the tissue.
Embedding – First job performed every morning, after cassettes are removed from the processor. Tissues are first transferred to an embedding mould according to the size and pressed down using a weight (to ensure that the tissue will be flat), and embedded with paraffin wax. Blocks are then put onto an ice block for cooling.
Shaving, Sectioning and Fishing – After the wax is hardened, blocks are shaved at 10µm using the microtome to first expose the tissue. This is followed by sectioning, where tissues are sectioned at 3µm. Sectioned tissues are first placed into cold water and fished using pencil-labeled slides before transferring into the water bath containing hot water (43-48 deg C), which expands the tissue to remove folds. A thermometer must be placed inside the water to ensure that the water is not too hot as this may damage the tissue. The orientation of the sections is also very important in fishing. If fished too high, the tissue may not be stained by the autostainer (reagents in the autostainer are only of certain volume). Slides will then be arranged in slide holders and placed into the oven for heating for 15 mins at 85 deg C to ensure tissues are properly attached onto the slides to prevent detachment/sliding off during staining. Tissues can be fished 6, 3, 2 or 1 in a slide according to the size (smaller tissues are fished more in a slide).
Staining – Slide holders removed from the oven is then immediately placed into the auto-stainer, which performs the H & E stain. Special stains such as PAS, iron and reticulin stain are performed manually. Different programs in the autostainer perform different procedures (eg. program 8 is used for H & E staining and program 7 is used for dehydration, for special stains). This machine is connected to an autocoverslipper, which automatically mounts coverslips on slides without producing bubbles. Many racks can be loaded into the autostainer at once, thus the use of this machine had saved a lot of time compared to manual staining.
Sorting – Slides stained will then be checked against the tissue blocks (to tally the size and shape of tissue) to ensure labels are pasted correctly before they are sent out to the pathologists, who make the diagnosis. Used blocks will be kept into boxes in ascending order to ensure easy retrieval when additional special stains or re-cuts are requested by pathologists.
Other Histopatological Aspects
Frozen Sections – This is done when immediate results are required, usually when an operation is still in progress. When the doctor removes any tissue and is unsure whether the surrounding tissues are affected, they will request for frozen sections. Once the histolab receives a frozen section request from the operating theater (OT), a medtech would have to rush to the specimen room located around the OT to collect the fresh specimen. The pathologist in charge should already be on stand-by in the lab. Once the specimen reaches the lab, the pathologist will carry out the trimming personally. The trimmed tissue will then be treated with liquid nitrogen and sectioned using the cryocut. This is followed by the manually performed rapid H & E staining and microscopic analysis by the same pathologist. They will then call the OT to report the results. The whole process (from the time when the specimen reaches the lab to the delivery of results) must be completed within 20 mins, thus it can be very stressful when performing this procedure.
Immunohistochemistry Stain – Commonly used in the diagnosis of abnormal cells such as those found in cancerous tumors, this type of stain is performed when the pathologist suspects any abnormality in the morphology of the H & E stained slides and requires confirmation. The stain exploits the principle of antigen-antibody reaction; using specific antibodies to detect the antigens present in the cells. Firstly, slides with the cut sections and cover tiles (to protect the tissue from any damage during the staining process) are loaded into the machine. Then tumor markers such as CD31, estrogen and CK-7, which are contained in containers, are added. Positive reactions with these markers can indicate particular cellular events such as proliferation or apoptosis. These positive results can be visualized based on enzymatic conversion of an added substrate (DAB) into a brown colored precipitate at the sites of antigen localization (ie. if cells stained appear brown, there is a positive antibody-antigen reaction).
Special Stains – These are done also as confirmatory tests for diagnosis. When the pathologists suspect an abnormality in the H & E stain, they will order for special stains. Some examples are PAS & PASD, GMS and TB and Prussian blue stain (I will only elaborate on PAS & PASD, cos this is the most commonly used test):
PAS (Periodic Acid Schiff’s) detects the presence of glycogen, fungus and mucin. It stains these components magenta (using Schiff’s reagent) and the nucleus blue (haematoxylin as counterstain). PAS is always done with PASD, which has the same protocol as PAS; only that it has an additional step of treatment with diatase, which deploys glycogen into smaller sugar units that can be washed out after treatment. Glycogen stained magenta on the PAS stained slide and will be absent on the PASD stained slide. This absence of glycogen will clearly show the presence of fungus and mucin.
I will be changing lab next week. But I havent seen post mortem case (autopsy of babies)! Cos there is none. Not that I'm a saddist, my supervisor say must see. Nvm, this might not be a bad thing.
Anyway that's all I have for now. Have fun =)
Ka Hang
TG02
Week 2 (30/6 - 4/7)
Week 1 (23/6 - 27/6)
There was some problem with my documents to start work at my research laboratory, so I had to stay in school for the first week to do research on flow cytometry to prepare me for my research work which will involve dealing with flow cytometry cell sorter... It's going to be an exciting SIP for me! hahaz.
Principle
It is a rapid technique that allows the analysis and identification of individual cells from a pool of heterogeneous sample population using multiple parameters.
Process of flow cytometry (Overview)
- Make a single cell suspension of the interested cell culture
- Use of antibodies bound with fluorochromes (PI) that is cell specific and incubate before washing (May involve use of multiple different specificity types of antibodies at any one time for flow cytometry)
- The sample is then loaded onto the flow cytometry
- Before using the flow cytometry, it is required to warm up the laser
- The sample is pressurized upwards or downwards depending on the type of hydrodynamic focusing used (sheath fluid is used to propel the sample into the flow chamber where the laser is located)
- The sample pass through the flow chamber where it is restricted to a single cell file flow
- A laser beam (normally an argon-ion laser is used) is focused on the cell flow, in the flow chamber, where cells with bound antibodies will have the fluorochromes attached excited into giving off light (depending on the type of flurorchromes used)
- The light scattered is collected by the orthogonal collection lens, which has a high numerical aperture for maximum fluorescence collection possible, to be measured by the photomultipliers where it is amplified and processed for analysis in the computer through digital conversion
- If the interested cell is identified, the flow chamber is charged at the moment of cell droplet formation (eg. Negative charged)
- The droplets are then pass through a pair of charged plates
- The charged plates function to deflect and collect different charged cell droplets
- The droplet with the interested cell is deflected towards the positive charged plate and collected into collection vessels for further analysis or use
Applications:
- Immunophenotyping
- Ploidy analysis
- Cell counting
- GFP expression analysis
Basic overview of the flow cytometry setup
The components are:
- Fluidics system
- Optics
- Signal detection and processing
- Electrostatic cell sorting (For flow cytometry equipped with cell sorting capabilities)
Fluidics system
It is a flow system that employs a concept of prssurized flowing fluid, shealth fluid, for single cell line presentation to the interrogation point and removes the waste into the waste container at the end of the flow.
Sheath fluid: usually an isotonic saline solution with the purpose of propelling the sample into the flow chamber.
The presentation of a line of single cells to the interrogation point is termed: hydrodynamic focusing

Figure 1.2: Hydrodynamic focusing of the sample core through a nozzle tip
Taken from: http://www.stemcell.umn.edu/img/assets/10061/Intro_to_Flow_Cytometry_Learning_Guide.pdf
Interrogation point
The point of intersection between the laser beam and the sample delivered in the flow chamber.
Optics
The system in the flow cytometry that is concern with manipulating the properties of light for signal detection and processing.
Light source
Blue light argon-ion laser = 488nm
UV laser = 360-380nm
Three main points:
- Light beam focusing
- Light collection
- Optical filters
Light beam focusing
Laser beam use optic lens to focus the intensity of the beam onto the sample stream where a cross-section of 50um laser beam is commonly set-up.
A flat-topped beam is commonly used for flow cytometry system in order to give a uniform lighting of the moving cells.
 Figure 2: Cross-sectioned laser beam focused by laser optics lens
Figure 2: Cross-sectioned laser beam focused by laser optics lensTaken from: http://biology.berkeley.edu/crl/flow_cytometry_basic.html
Light collection
The collection lens is required to have a high numerical aperture value for maximum collection of the low fluorescence and other light signals from cells.
Optical filters (Not important)
Not use for monochromatic light from lasers. They are used for arc lamp that requires filtration to give the right excitation light wavelength for appropriate fluorescent dyes; however, these are rarely used now.
Signal detection and processing
Signal detection
There are three types of light to be detected by a light detector:
- Forward scatter light (also known as low-angle light)
- Side scatter light
- Fluorescent signals
Forward scatter light
The measurement of the degree of forward scatter light is approximately proportional to the cell size. Therefore, the larger the cell, the larger the degree of forward scatter light detected.
These can be used to differentiate cells with different cell sizes:
- Red blood cell (6um)
- Lymphocyte (8um)
- Neutrophil (12um)
- Monocyte (14um)
 Figure 3: Picture of a forward scatter light detector with an obscuration bar in front on the right side of the picture
Figure 3: Picture of a forward scatter light detector with an obscuration bar in front on the right side of the pictureTaken from: http://probes.invitrogen.com/resources/education/tutorials/4Intro_Flow/player.html
Side scatter light
The measurement of the degree of the side scatter light signal is approximately proportional to the granularity and structural complexity intracellularly.
These can be used to differentiate cells with varying granularity and structural complexity:
- Lymphocytes (low intracellular complexity)
- Monocytes (higher intracellular complexity)
- Granulocytes (highest intracellular complexity)
 Figure 4: Picture of a side scatter light from a cell
Figure 4: Picture of a side scatter light from a cellTaken from: http://probes.invitrogen.com/resources/education/tutorials/4Intro_Flow/player.html
Fluorescent signals
These involve the use of antibodies coupled fluorescent molecules that are excited with the right laser wavelength in the flow cytometry and gives off a fluorescence signal.
Types of Fluorochromes used (excitation at 488nm):
Label Proteins:
Fluorescein Green color
R-phycoerythrin (PE) Orange color
Phycoerythrin-Texas Red conjugate (ECD) Red color
Phycoerythrin-cyanine5 conjugate (Cy-chrome) Deep red
Conjugated peridinin chlorophyll (PerCP) Deep red
Label DNA:
Propidium iodide (PI) Red color

Figure 5: Fluorescent dyes and their properties
Taken from: http://www.ab-direct.com/uploads/Flow-Cytometry.pdf
Optical filters
They are dichroic filters which are used for detection of many signals simultaneously.
Dichroic filters acts as a filter and a mirror: allows light wavelength of specific length to pass through while reflect the remaining blocked light to specifc light detectors.
There are three types of dichroic filters:
- Long pass filter
- Short pass filter
- Band pass filter
Long pass filter
Blocks light below cut-off wavelength and transmit the light above that specific wavelength.
Short pass filter
Blocks light above cut-off wavelength and transmit the light above that specific wavelength.
Band pass filter
Block light below and above a certain specific cut-off wavelength and transmit the light from that narrow wavelength.

Figure 6: Diagram of the properties of different filters (shaded area is the light wavelength allowed to be transmitted through the filter)
Taken from: http://probes.invitrogen.com/resources/education/tutorials/4Intro_Flow/player.html
Signal processing
The lights detected from the each of the light detectors are converted into voltage pulse and this data is transfer into a computer program to be analysis.
Taken from: http://www.ab-direct.com/uploads/Flow-Cytometry.pdf
Electronics and peripheral computer system
As the light signals detected are normally too small to be plotted on a graph, they have to be amplified first. These are done by a chain of linear or logarithmic amplifiers in a computer program before plotted on a graph, histogram.
There are three types of amplification:
- Logarithmic amplification/scaling
- Linear amplification/scale
- Biexponential amplification/scaling
Logarithmic amplification
It amplifies weak signals and constricts strong signals so that they are evenly distributed to be plotted on a histogram. It is commonly used for fluorescence analysis.
Linear amplification
Unlike logarithmic amplification, linear amplification is used for a narrow range of signals so that the data could be seen clearly on the histogram. It is commonly used for DNA studies.
Biexponential amplification
It is a combination of logarithmic and linear scale at the upper end and lower end respectively which is also used on the graph for flow cytometry.
Taken from: http://probes.invitrogen.com/resources/education/tutorials/5Data_Analysis/player.html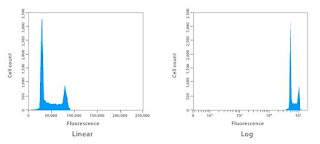
Taken from: http://probes.invitrogen.com/resources/education/tutorials/5Data_Analysis/player.html
Electrostatic cell sorting
This is an extended function of flow cytometry with the capabilities to sort the cells according to the data inputted into the computer system on the cells of interest as the selection criteria.
This application consists of three parts:
- Droplet formation
- Droplet charging
- Deflection plate (voltage plates)
Droplet formation
It is important to form droplets of approximately equal sizes to achieve only the formation of droplets which only contain one cell each for the purpose of accurate cell sorting. This is done through the high vibration of the nozzle part in the fluidics system where the fluid exits.
Droplet charging
When the droplet which contain the single cell of interest which fits the selection criteria. The fluid stream is charged at the precise ‘break-off point’ during the droplet formation.
Break-off point
It defines the moment where the droplet contains the cell of interest is formed and detaches from the fluid stream.
Deflection plate
After the charged droplet containing the cell of interest is release from the fluidics system and drip down towards the compartment containing the plates where it will be deflected left or right, depending on the charge. Non-charged droplets will just drip down into the waste container located right below the nozzle.

Figure 10: Diagram of the process of electrostatic cell sorting based on droplet charge
Taken from: http://www.ab-direct.com/uploads/Flow-Cytometry.pdf
(OH and ya, I absolutely hate blog posting, cause I am a blog idiot..! Posting a blog is such a frustrating task!
If only they have an attachment file tab, then I could attach microsoft word directly to each posting instead of spending my time trying to organise my documents which never fail to end up in a mess after I copy pass from my microsoft word document!!!)
Reference List:
1. Misha Rhaman. (2006). AbD SEROTEC. Introduction to Flow Cytometry. Retrieved June 29, 2008, from http://www.ab-direct.com/uploads/Flow-Cytometry.pdf
2. Nicoll, A. K. (2004). University of Dundee. SLS Flow Cytometry Core Facility: What is Fluorescent Activated Cell Sorting (FACS)? Retrieved June 29, 2008, from http://www.dundee.ac.uk/lifesciences/FACS/cell_sorting.htm
3. Invitrogen. (2008). Introduction to Flow Cytometry. Retrieved June 29, 2008, from http://probes.invitrogen.com/resources/education/tutorials/4Intro_Flow/player.html
4. Invitrogen. (2008). Data Analysis for Flow Cytometry. Retrieved June 29, 2008, from http://probes.invitrogen.com/resources/education/tutorials/5Data_Analysis/player.html
5. BD Bioscience. (2000). Introduction to Flow Cytometry: A Learning Guide. Retrieved June 29, 2008, from http://www.stemcell.umn.edu/img/assets/10061/Intro_to_Flow_Cytometry_Learning_Guide.pdf
By: Low Quan Jun 0607243C TG02 (Post: 29 June 2008 Edited: 04 July 2008)
