Before that, do you know how specimens reach the lab? All along I thought they were sent in by some medical staff every now and then. But one day when I was helping out at the reception, I realised it was not. The specimens are received in the lab via a pneumatic transport system (that looks like water pipes) that is linked from every single ward or clinic to the lab. Samples from the wards to be sent to the lab are placed into a capsule, which contains a micro-chip that is recognised by the system to direct its way to its destination. In every ward or clinic, there will be this cupboard that contains the ‘pipe’. Empty capsules with reports from the lab (if available) will then be sent back to the respective wards using the same system. But because there is only one lane for sending out, the destination code must be keyed to ensure that they are sent back to the correct place. Isn’t this interesting? The WHOLE hospital is connected by all these ‘pipes’.

Capsules arriving from wards
 Capsules waiting to be sent back to clinics/wards
Capsules waiting to be sent back to clinics/wards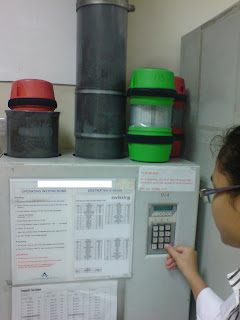
Sending back capsules with reports through the one and only lane
(destination code keyed)
Ok, back to haematology. ESR (Erythrocyte Sedimentation Rate) is one of the most common tests performed in the haematology lab. There are many ways to test for the ESR. In my lab, the sedi-rate P4-Micro System is used. It measures the rate at which red cells fall in the first 50 mins when anti-coagulated blood is allowed to stand. Red cell sedimentation occurs in 3 stages: in the preliminary stage where aggregates form within a few minutes. This is followed by a period of time in which the sinking of the aggregates takes place at a constant speed. Finally, as the aggregated cells pack together at the bottom of the test tube, sedimentation rate slows down.
ESR is used to help diagnose conditions associated with acute and chronic inflammation. When inflammation is present in the body, certain proteins cause red blood cells to stick together and fall more quickly than normal to the bottom of the tube. These proteins may be produced when there an infection, autoimmune disease, or cancer. However, ESR is said to be nonspecific because increases do not indicate the exact site of inflammation or the causative agent. For this reason, a sedimentation rate is done in conjunction with other tests to confirm a diagnosis. Once a diagnosis has been made, a sedimentation rate can be done to help check on the disease or see how well treatment is working.
To perform ESR:
2. Then, a thin pipette is being pushed downwards into the tube, until the blood fills the whole pipette, indicated by the ‘0’ marking.
3. Next, the tube with pipette will be allowed to stand.
4. Exactly after 50 mins, the number of mm the red cells fallen would be read.
5.Results are then recorded in the ESR record book and the request form, and entered manually into the LIS.
 Source taken from: http://www.globescientific.com/sedirate™-autozero-westergren-esr-system-3469-pi-574.html
Source taken from: http://www.globescientific.com/sedirate™-autozero-westergren-esr-system-3469-pi-574.htmlFoetal RBCs contain mainly HbF (a2g2). They resist acid elution more than that of adult RBCs, which contain mainly HbA (a2b2). With this principle, foetal cells can take up the eosin when counterstained and appear as darkly stained red cells. On the other hand, adult cells will be disintegrated by the acid and therefore will appear as ghost cells (because the cells are dissolved, there is no more cells present to take up the stain).
To perform the KB test:


.bmp) Note: The display of some acquisition dashboard might vary a little, but they all basically have the same functions.
Note: The display of some acquisition dashboard might vary a little, but they all basically have the same functions.




.bmp)




